Because the condition can be confusing, here’s some information behind disc herniations and disk degeneration.
What are spinal discs?
The word “disc” is a bit of a misnomer, as spinal discs are actually rubbery pads located between the vertebrae, the bones that make up the spinal column. Each disc is a flat, circular capsule about an inch in diameter and one-quarter inch thick. They have a strong, fibrous, outer membrane and an elastic core. In Dunkin’ Donuts terms, you could think of a disc as similar to a jelly donut.
You’ve heard the term “slipped disc,” but there isn’t really much room for the discs to move. They are firmly embedded between the vertebrae and are held in place by the ligaments connecting the spinal bones and the surrounding sheaths of muscle.
You’ve probably also heard the discs described as the shock absorbers for the spine, but this gives them the characteristic of being softer and more pliable than they really are. They are only soft in children when they are gel. By the time a person becomes an adult, the blood supply to the discs has stopped and the soft inner material is hardening. By middle age, the discs are tough and non-malleable, similar to a circle of hard rubber.
This is where the trouble comes in because as the discs become harder the protective lining becomes weaker and the discs are more prone to injury.
Herniated discs
So, what happens when a disc “herniates?” This is the word used when the disc’s inner material swells and pushes through the outer membrane. Or the disc can become distorted and bulge in spots (you’ve heard “bulging disc”). The inner core then protrudes and can press against surrounding nerves. If this happens and you keep pushing things the membrane can rupture or tear, allowing the inner disc material to push out further causing extreme pain. This is a herniated disc.
This happens predominantly in the lower back, rarely occurring in the cervical spine. Sometimes, the herniated disc doesn’t press on the nerves and the person won’t feel pain. Herniated discs are most common between the ages of 30 and 50. Because their discs no longer have fluid cores, older people are much less likely to have a herniated disc. At least this is one good thing about getting older!
What causes a herniated disc?
The term herniated disc sounds relatively violent, and they can result from a violent injury. But more often they are a result of normal aging combined with everyday activities such as lifting a heavy object the wrong way or over-extending in a sport. Sudden moves, such as making a cut in a Turkey Bowl game or missing a step on a stair, can also herniate a disc.
What can you do to prevent a herniated disc?
What you want to do is strengthen the muscles that support the spine. Regular, moderate exercise can prevent many of the issues that cause a herniated disc. Flexibility is also a plus. People who are more sedentary are more likely to have disc problems. Carrying excess weight also puts more stress on the spine, making disc herniation more likely.
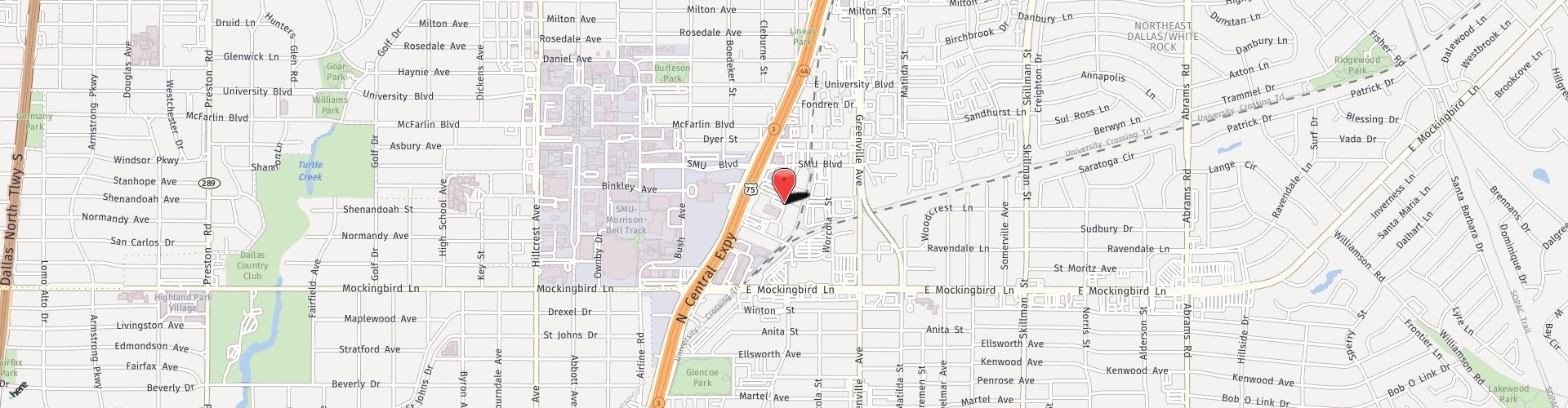
Are you suffering from back pain? Call us at Texas Neurosurgery, (214) 823-2052, and come see us at our new Dallas office. We can get you past the pain.